Health professions educators are often unconsciously competent in the work they do. This means it is often difficult for these educators to think about what they are doing and why and explain that to their learners. It takes intentionality and practice to make unconscious thinking conscious and transparent.
What is transparent thinking? In education it has been called “think-aloud,” or modeling with explanation. It is when the educator intentionally talks about what they are doing and why when modeling and explaining a task, procedure, conversation, or thought process.
Types of Transparent Thinking
There are three different and interconnected ways health professions educators need to be transparent when teaching: clinical modeling, teaching relevance, and teaching pedagogy.
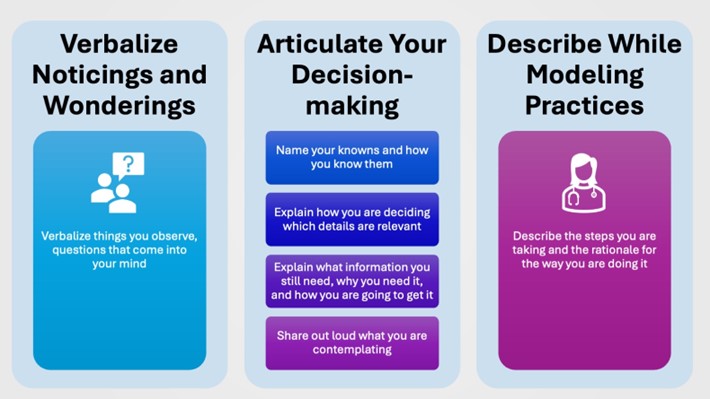
Transparent Clinical Modeling: Excellent health professions educators model actions and thought processes while simultaneously explaining what they are doing why. As described in the image below, when engaging in transparent thinking about clinical thought processes or clinical reasoning, there are three ways to engage learners described.
Clinical modeling and transparent thinking can take place while modeling the following:
- Tasks: reviewing charts, calling codes, using equipment
- “When you log into the EMR first you want to...”
- “If a patient... then you call the code by...”
- Procedures: suturing a wound, taking a blood pressure, starting an IV
- “I do it in this way because...”
- “Next I would... because...”
- Conversations: counseling patients, giving bad news, reconciling medicines
- “When I am giving families bad news I…. because….”
- “I always start a smoking cessation conversation with… because…”
- Clinical Reasoning: interpreting labs, deciding further tests, deciding on a treatment plan
- "When I see these lab results, I am thinking... because...”
- "Because the patient is presenting... I want to order... because...”
Transparent Teaching of Relevance: Explain what you are teaching and why it matters that your learners learn it. Health professions students are adult learners, and they learn best when content is relevant, meaning they know why they need to learn it for their own growth. Working to be transparent, educators will be motivated to re-evaluate relevance and refer to course or programmatic outcomes when communicating relevance.
- “You will need to know this when…”
- “When a patient has… you will need to know…”
- “If you do not know how to… then you will not be able to effectively…”
Transparent Teaching of Pedagogy: Explain why you are teaching something in a certain way. In health professions education learners are always a teacher to the next generation. Therefore, it is important to label and explain the teaching moves you make so that your learners can replicate the same things with their learners. Additionally, learners are often unaware when they are being taught or provided feedback, so it is important to “signpost” it for them.
- "I am going to do some teaching today. First, I will… because… then I am going to ask you to… because…”
- “I am going to observe you and watch how you… because… then I am going to give you some feedback and some pointers.”
- “I am first going to demonstrate how to do this procedure and explain what I am doing and why because... Then I want you to try it while I tell you what to do and why.”
Become Consciously Competent and Pass the Baton
To enhance educator effectiveness in health professions, fostering transparent thinking is pivotal. By transitioning from unconscious competence to conscious competence through metacognitive practices, educators can cultivate a reflective mindset. This entails posing guiding questions, envisioning desired student cognitive development, and facilitating student inquiry. Ultimately, the goal is to pass the baton, empowering learners to articulate their thought processes and engage in tasks autonomously.
#MedEdPearls are developed monthly by the Health Professions Educator Developers on Educational Affairs. Previously, #MedEdPearls explored topics including making teaching stick, questioning, and optimizing the clinical learning environment.

Stacey Pylman, PhD, is Assistant Professor and Director of Continuing Medical Education in the Office of Medical Education Research and Development (OMERAD) at Michigan State University College of Human Medicine. Her areas of professional interest include debriefing early clinical experiences, effective teaching in medical education, and instructional coaching. Stacey can be followed on Twitter or contacted via email.
#MedEdPearls

Jean Bailey, PhD – Virginia Commonwealth University School of Medicine
Rachel Moquin, EdD, MA – Washington University School of Medicine

