Purposeful questioning starts with understanding the reasons educators ask learners questions. There are three reasons educators ask questions 1) to scaffold learning, 2) to evaluate, or 3) to challenge thinking.
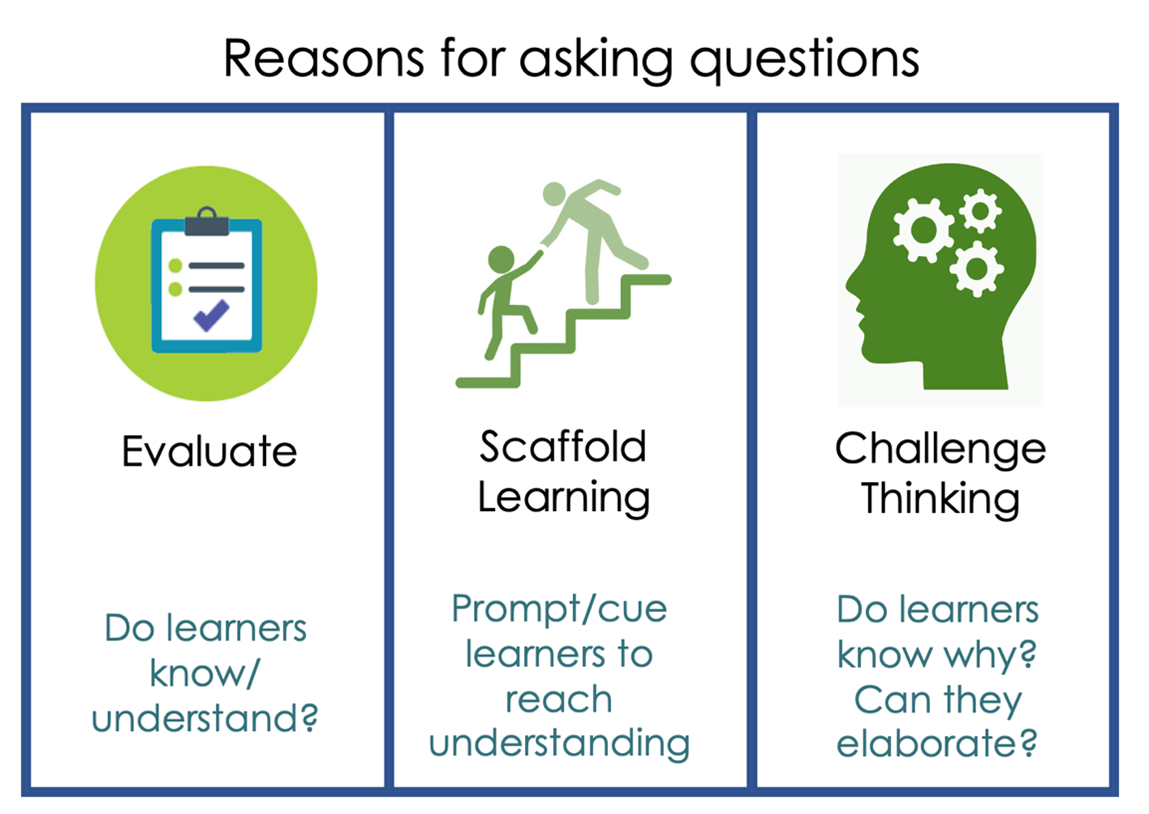
Scaffold Learning: Scaffolding is a dynamic process that requires the educator to be able to identify the knowledge gap faced by a learner and then offer support for the learner as they fill the gap and move toward a more advanced understanding. To do this well, the educator must have two ideas in mind: the learning objective and the learner’s current level of knowledge. Asking questions to scaffold learning in the clinical setting is often done in the moment through a give and take between the learner and educator.
Consider the following when designing questions:
- What do my learners already know about this topic?
- What do I want my learners to know about this topic when they leave?
- What questions can I ask that will help learners think and fill in knowledge gaps?
The trick is to ask questions that help learners access what they do know and build from there with further questions as guides. For example, in the following segment the medical educator uses questions to scaffold the learner to understand how bacterial middle ear infections occur:
Educator – These microbiotas are common in the respiratory tract so why doesn’t everyone get an ear infection?
Learner – I don’t know…
Educator – So think about it, why do we have a eustachian tube?
Learner – To drain the ear.
Educator - Yes to drain the middle ear. But what happens to this space once the eustachian tube gets blocked with fluid and pathogens?
At the start of that discussion, the learner is unable to answer the question asked. However, the medical educator scaffolds thinking to support learning to this next level.
Evaluate: Questioning is most often thought of as a way to assess or evaluate what learners know, and it is effective in doing so. It can be used to assess understanding, clinical skills, and reasoning to promote learner progress toward independence in the clinical setting. When educators have a clear understanding of what learners know and what they need to know (learning objectives), they can ask questions to help learners bridge knowledge gaps.
Challenge Thinking: Lastly, questions can be asked to challenge student thinking. When asking questions for the purpose of challenging, the educator might ask the learner to elaborate on their answer, ask if the learner knows why, or ask the learner how it might be different if a variable was changed. Still, caution must be used when asking learners challenging questions. It is important to explain to students the purpose(s) for asking the questions and to have already developed a safe learning environment.
When asking questions while teaching, your purpose for asking the question should align with the types of questions you are asking. Make sure you and your students understand your purpose for asking the question. Explicitly state, “I am asking you this question to challenge your thinking.”
For more tips on effective questioning check out Pylman and Ward 2020, Amin and Khoo 2003, or Kost and Chen 2015.
#MedEdPearls are developed monthly by the Health Professions Educator Developers on Educational Affairs. Previously, #MedEdPearls explored topics including question bursts, questioning to assist in supervision levels and EPAs, and assessing clinical reasoning.

Stacey Pylman, PhD is an Assistant Professor in the Office of Medical Education Research and Development (OMERAD) at Michigan State University College of Human Medicine. Her areas of professional interest include debriefing early clinical experiences, effective teaching in medical education, and instructional coaching. Stacy can be followed on Twitter or contacted via email.
#MedEdPearls

Jean Bailey, PhD – Virginia Commonwealth University School of Medicine
Rachel Moquin, EdD, MA – Washington University School of Medicine

