The medical practice landscape has changed towards a more team-oriented and inter-professional approach. Physicians are expected to function as effective members of multidisciplinary teams, as the patient case mix has increased in complexity, chronicity and age. Developing collaborative skills in medical education is essential as medical students will enter a dynamic world of team-based medical practice. Therefore, teamwork training is a requisite in medical school to nurture appropriate competencies in the physicians of the future. The literature recommends beginning collaborative and teamwork training at the start of medical training, using implicit team learning (e.g. problem based learning and team based learning activities where students work interdependently to achieve learning outcomes while teamwork/collaboration is influenced by the facilitator) for early students and progressing towards more explicit team learning (e.g. clinical simulation activities where students work interdependently and are given explicit instruction and practice in teamwork/collaboration with the goal of improving their performance) as students advance.
Promoting collaborative learning in medical students was an area of my medical education doctoral research. During this research, I explored medical students’ participation in an array of small group collaborative learning activities as they progressed through the different stages of becoming a doctor. As the students progressed from the basic sciences to more clinical work, the repertoire of activities increased from more in-class collaborative learning towards interprofessional and workplace collaborative learning in clinical contexts. There was a considerable overlap between the different collaborative learning activities. Upon entering a medical school, students usually began to participate in peer learning activities in a small group which were formal (e.g. problem-based learning, team-based learning, case-based learning) and/or informal (e.g. study groups). In the next stage as students began to attend clinical sessions and ward rounds, they experienced more Interprofessional learning and collaboration. Interns and residents become active members of the clinical teams in the workplace context and in this stage, there was a focus on a practice-based approach to learning collaboration and teamwork skills. I found that the different stages of developing the collaborative learning and teamwork competency can be organized on a continuum depicting the gradual transition of learning and working contexts in which medical students sequentially participate and develop their collaborative learning skills. However, the sequence of stages may vary depending on different contexts and cultures of the medical school.
The diagram presents my conceptualization of the literature on how medical students participate in different learning contexts, along with the range of opportunities in which they can develop their skills in collaboration and teamwork across medical education.
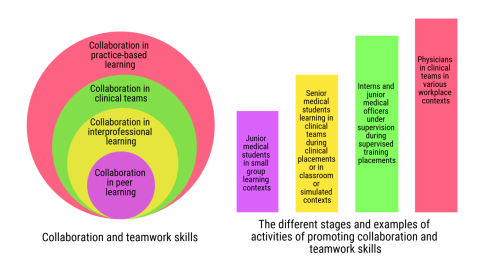
Figure: Continuum of collaborative learning in medical education and clinical practice
How can medical students be supported to develop their collaboration and teamwork skills?
Here are some suggestions:
- Establishment of group work early in medical education is important, as it allows students to participate and learn together. Students benefit from participation in both formal and informal small group collaborative learning activities designed to encourage communication, interaction, learning and working together towards a common goal.
- Guided participation can aid students to effectively learn and interact in collaborative learning environments. This guidance can encourage successful transition both in terms of adapting to the profession and new ways of learning.
- Use of educational instruments which have been developed to both evaluate students and serve as bases for providing formative feedback on important competencies. A suite of workplace-based assessment tools has been designed to evaluate collaborative skills and participation in teamwork in the clinical context. Formative assessment instruments used in the workplace coupled with feedback have been effective in changing the behavior of learners. Examples of instruments used in the clinical context include the Professionalism Mini-Evaluation Exercise (P-MEX) and the Teamwork Mini-Clinical Evaluation Exercise (T-MEX).
How do you promote effective collaborative learning in your students? What strategies have you designed to enhance the collaborative and teamwork competency in your students? Please share your experiences by commenting below!
Did you know that the Harvard Macy Institute Community Blog has had more than 200 posts? Previous blog posts have explored topics including team science principles in academic medicine, drive theory, and interprofessional education.
Author BIO

Maha Pervaz Iqbal, MBBS MMeD (Dundee) PhD (UNSW) AFANZAHPE [Leaders ‘19]. Maha works as a medical educator at the Faculty of Medicine, University of New South Wales. Her research interests include educational innovation and teamwork and leadership in medical education. Maha can be followed on Twitter or contacted via email.
Maha Pervaz Iqbal

Maha Pervaz Iqbal, MBBS MMeD (Dundee) PhD (UNSW) AFANZAHPE [Leaders ‘19]. Maha works as a medical educator at the Faculty of Medicine, University of New South Wales. Her research interests include educational innovation and teamwork and leadership in medical education. Maha can be followed on Twitter or contacted via email.

